Enter the patient's diagnostic and treatment details in Electronic Health Record (EHR)?
In this step, providers are tasked with gathering all the information required by payers to process the payment. EHR or Electronic Health Record contains patients' medical history and automates the workflow for the providers. Document the complete diagnosis examination results and treatment plans for optimal reimbursement.
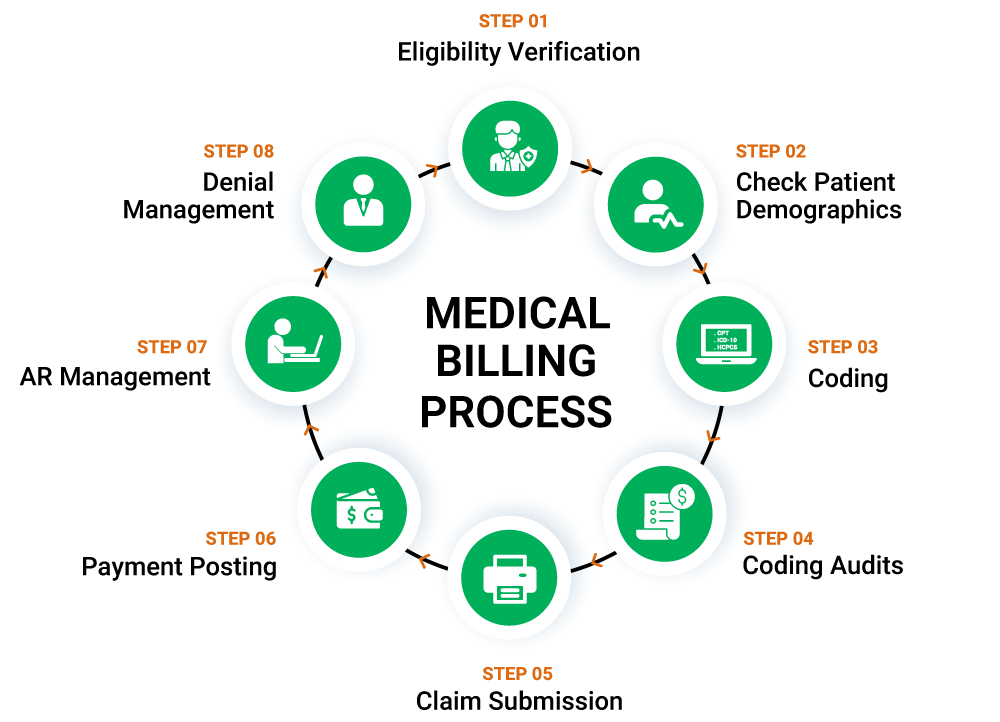
Claims Submission
Before the claim is submitted, it needs to be checked for any errors. Legion Medical Billing service providers can work in tandem to deliver maximum reimbursement. For the first transaction, the claim for all the services provided by the provider is known as X12-837 or ANSI-837. This document contains large amount of patient data, the interaction between patient and provider, and references info about the provider. The payer responds with X12-997, this is a simple acknowledgment with regards to claim submission. X12-835 transaction describes the items that will be paid or are denied. If paid, the amount is mentioned, and if denied, the reason.