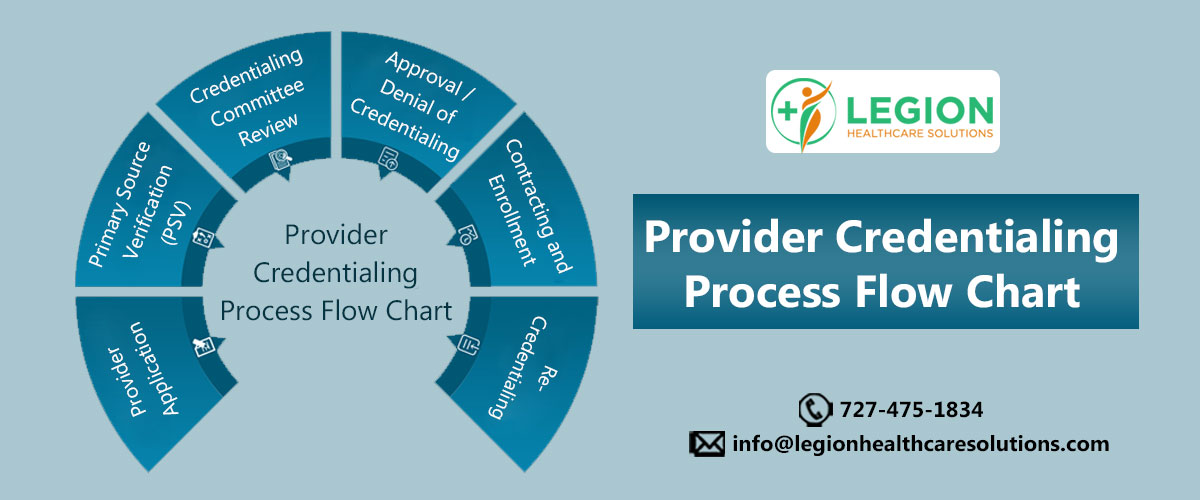
Provider Credentialing Process Flow Chart
Provider credentialing is a critical process in the healthcare industry, which involves the verification of a healthcare provider’s credentials, qualifications, and experience to ensure they meet certain standards set by the insurance companies. The provider credentialing process flow chart is a critical tool that can help healthcare providers by streamlining the credentialing process and ensuring that they meet the necessary qualifications to provide quality healthcare services to patients. By following the flow chart, healthcare providers can understand the steps required to complete the credentialing process and prepare for the information and documentation needed to complete their application.
Step 1: Provider Application
The healthcare provider interested in joining the network completes an application and submits it to the healthcare organization or insurance company. The provider completes an online application and attaches all requested supporting documents containing data on their work history, education, references, and more. The application also includes instructions for the provider on what to list and how far back to go when detailing their history. The credentialing or enrollment professional’s role is to follow up until all necessary data and documentation is received, with provider data management software used to keep both parties on track.
Step 2: Primary Source Verification (PSV)
The healthcare organization or insurance company verifies the accuracy of the information provided by the provider through Primary source verification (PSV). Primary source verification is the act of going directly to the issuer of the data or certificate to verify credentials, either before or after a completed application is received, depending on the healthcare organization’s policy and protocol. Another organization may act as an agent for the primary source in providing information for PSV.
PSV is critical to the credentialing process, as it helps to identify impostors or individuals who exaggerate or fabricate professional qualifications to gain access to patients, creating significant risk. Credentialing and enrollment professionals must be vigilant in conducting PSV, as they often operate with limited staff resources and under strict time constraints to on board providers quickly, so hospitals can serve patients and receive payment.
Step 3: Credentialing Committee Review
The credentialing committee carefully reviews the provider’s application and accompanying documents to ensure that they meet the insurance company’s standards and requirements for credentialing. The committee may conduct additional background checks and review any red flags identified during the primary source verification process before making a recommendation to either approve or deny the provider’s application. This step ensures that only qualified and competent providers are granted privileges to practice within the healthcare organization.
Step 4: Approval/Denial of Credentialing
The credentialing committee reviews the provider’s application and accompanying documents and makes a recommendation based on the provider’s qualifications, compliance with industry standards and regulations, and other relevant information. Then the insurance company’s internal committee may make the final decision or may submit their recommendation to an external accrediting organization for review. The accrediting organization may review the recommendation and make a final decision on behalf of the insurance company.
If the provider’s application is approved, they become part of the insurance company’s network of providers and are eligible to receive reimbursement for services provided to patients with insurance coverage. If the application is denied, the provider may have the opportunity to appeal the decision through the insurance company’s appeals process.
Step 5: Contracting and Enrollment
If the provider is approved for credentialing, the insurance company will typically enter into a contract with the provider and enroll them in their network. The contracting process involves negotiating the terms and conditions of the agreement between the provider and the insurance company. This may include negotiating reimbursement rates, contractual obligations, and other terms of the agreement. The contract serves as a formal agreement between the provider and the insurance company, outlining the rights and obligations of both parties.
Enrollment is the process of adding the provider to the insurance company’s network of providers. This involves updating the provider’s information in the insurance company’s provider directory and other databases, so that patients can easily find and access the provider’s services. During the enrollment process, the insurance company may also verify the provider’s credentials and ensure that they are in compliance with regulatory and contractual requirements. This includes verifying that the provider has active licensure and certifications, has not been excluded from federal or state healthcare programs, and is not subject to any sanctions or disciplinary actions.
Once the contracting and enrollment processes are complete, the provider is officially part of the insurance company’s network and can begin providing services to patients with insurance coverage. The provider is responsible for complying with the terms of the contract, including billing and coding requirements, quality assurance standards, and other contractual obligations.
Step 6: Re-Credentialing
Re-credentialing is the process of periodically reviewing and verifying a provider’s credentials to ensure that they continue to meet the insurance company’s requirements for participation in their network. Providers are typically required to go through the credentialing process on a regular basis, usually every two to three years, to ensure that they continue to meet the organization’s or company’s credentialing standards.
During the re-credentialing process, the insurance company may review the provider’s professional qualifications, work history, malpractice history, and other relevant information. The re-credentialing process typically involves sending the provider a re-credentialing application, which they must complete and submit along with any required supporting documentation. The insurance company may also conduct a site visit or interview with the provider to verify their credentials and ensure that they are in compliance with contractual and regulatory requirements.
Once the re-credentialing process is complete, the insurance company will either approve the provider for continued participation in their network or deny their application. If the provider is denied, they may have the opportunity to appeal the decision or take steps to address any deficiencies that were identified during the re-credentialing process.
The provider credentialing process flow chart provides transparency in the process, ensuring that providers are informed of the status of their application and any issues that need to be addressed. Ultimately, the flow chart helps providers navigate the credentialing process with greater ease and efficiency, allowing them to focus on providing high-quality care to their patients.
About Legion Healthcare Solutions
Legion Healthcare Solutions is a leading provider credentialing service provider that specializes in assisting providers with complete steps of credentialing process. With years of experience in the industry, Legion Healthcare Solutions has a team of knowledgeable and experienced credentialing professionals who understand the intricacies of the credentialing process and work tirelessly to ensure that all providers meet the necessary standards for participation in a healthcare network.
As a trusted provider credentialing service provider, Legion Healthcare Solutions has built a reputation for excellence, reliability, and exceptional customer service, making them the go-to choice for healthcare providers looking to streamline their credentialing process. To know more about our credentialing and enrollment services, contact us at 727-475-1834 or email us at info@legionhealthcaresolutions.com
