Streamlining Your Practice: A Comprehensive Guide to Cardiology Medical Billing
Are you a cardiology physician in the USA looking to optimize your medical billing process? As a healthcare provider, navigating the complexities […]
Mastering Timely Filing CO 29 Denials: Strategies and Solutions
In the realm of medical billing, timely filing denials can be a significant challenge, particularly when it comes to CO 29 denials. […]
Navigating the Complexities of Medicare and Medicaid Reimbursement for Pain Management Services
Medicare and Medicaid reimbursement for pain management services can be a maze of rules and regulations, often leading healthcare providers to encounter […]
Unveiling the Importance of Addressing Old AR in Pain Management Billing
In the realm of pain management billing, addressing old accounts receivable (AR) is essential for maintaining financial health and maximizing revenue potential. […]
Optimizing SNF Billing: Strategies to Identify and Address Revenue Leakages
In the realm of skilled nursing facility (SNF) billing, revenue leakages can significantly impact the financial health of healthcare providers. Identifying and […]
The Vital Role of Choosing the Right Medical Billing Software and Outsourcing Services for Physicians
In the fast-paced world of healthcare, efficient medical billing is crucial for the financial health of medical practices. With the ever-changing regulations […]
Decoding Cardiology: A Comprehensive Guide to Common CPT Codes
In the realm of cardiology, understanding the nuances of CPT codes is essential for accurate billing and coding practices. Whether you’re a […]
Demystifying Medicare Crossover Claims: A Comprehensive Guide for Healthcare Providers
Medicare crossover claims are an integral part of the medical billing process for healthcare providers who treat Medicare beneficiaries. In this comprehensive […]
Mastering Internal Medicine Billing: A Comprehensive Guide for Physicians
Internal medicine billing plays a crucial role in the financial health of medical practices, yet it can be complex and challenging to […]
Unlocking Efficiency: The Benefits of Outsourcing Medical Billing Services
In the rapidly evolving landscape of healthcare, medical practices are constantly seeking ways to streamline operations, reduce administrative burdens, and maximize revenue. […]
Understanding CPT Code 99214 for Maximum Reimbursement
In the realm of medical billing, CPT code 99214 holds significant importance, particularly for healthcare providers offering evaluation and management (E/M) services. […]
7 Revenue Cycle Concerns for Pain Management Practices and Practical Solutions for Success
In the realm of pain management, ensuring a healthy revenue cycle is essential for the financial well-being and sustainability of practices. However, […]
Navigating Cardiology Billing Denials: Proven Strategies for Revenue Recovery and Practice Success
In the fast-paced world of cardiology billing, denials can pose significant challenges, impacting practice revenue and hindering financial stability. However, with the […]
How Outsourcing Family Practice Billing Can Transform Your Practice?
In the dynamic landscape of healthcare, family practice physicians face a multitude of challenges, from delivering quality patient care to navigating complex […]
Optimizing Accounts Receivable (AR) in Family Practice: Strategies for Corrective Action
In the complex ecosystem of a family practice, managing accounts receivable (AR) efficiently is vital for maintaining financial health. As physicians navigate […]
Step-by-Step Guide of Prior Authorization for MRI
Navigating the prior authorization process for medical procedures can be a complex and time-consuming task for healthcare providers. When it comes to magnetic resonance imaging (MRI), obtaining prior authorization is crucial to ensure seamless access to this valuable diagnostic tool.
Need of Professional Medical Provider Credentialing Services
As healthcare regulations and insurance requirements continue to evolve, the task of provider credentialing and enrollment becomes increasingly complex and time-consuming. This is where professional medical provider credentialing services, such as those offered by Legion Healthcare Solutions, come to the rescue.
Streamline Your Physical Therapy Practice: Experience the Benefits of Outsourcing Medical Billing to Legion Healthcare Solutions
Running a successful physical therapy practice requires a delicate balance between providing excellent patient care and managing administrative tasks. One aspect that often poses challenges is medical billing.
Streamline Your Pain Management Billing with Legion Healthcare Solutions
Pain management practices play a crucial role in enhancing patients’ quality of life, but billing and coding can often become a complex and time-consuming process.
A Comprehensive Guide to Prior Authorization with Aetna
Aetna, one of the leading healthcare insurance providers, implements a prior authorization process to determine coverage for certain medical procedures, medications, and services.
Understanding CPT Code 11042 – A Comprehensive Guide
CPT Code 11042 is an important code used in the medical field for billing and documentation purposes. It relates to the debridement (removal) of skin and subcutaneous tissue involving a single wound.
Medicare Chiropractic Billing Guide – Simplifying Reimbursement for Chiropractic Services
In this article, we will explore into the Medicare chiropractic billing guide, highlighting key points from the Centers for Medicare & Medicaid Services (CMS) to streamline the billing and coding process.
Streamline Your Practice with Professional Podiatric Medical Billing Services
In today’s complex healthcare landscape, podiatrists face numerous challenges in managing their practices efficiently while ensuring accurate and timely billing and reimbursement.
Coding OB GYN: An Overview for Gynecologist
Coding OB GYN can pose challenges for healthcare providers, making it crucial to understand the coding guidelines, common mistakes, coding scenarios, and commonly used codes in this field. In this blog, we will explore these key aspects, aiming to enhance your OB GYN coding and optimize your billing process.
Legion Can Help in Streamlining Provider Enrollment with BCBS
Legion Healthcare Solutions is here to support healthcare providers by offering comprehensive provider credentialing services. In this article, we will explore, how Legion can assist healthcare providers in their provider enrollment process.
CPT Code 99396 – A Comprehensive Guide for Primary Care Providers
Understanding CPT code 99396 and its associated guidelines is crucial for accurate medical billing and reimbursement. So, let’s dive into the details of CPT code 99396 and explore its importance in primary care practices.
A Healthcare Provider’s Guide to Prior Authorization with Cigna
As a healthcare provider, understanding the prior authorization process with Cigna is crucial in ensuring your patients receive the necessary coverage for their healthcare services and medications.
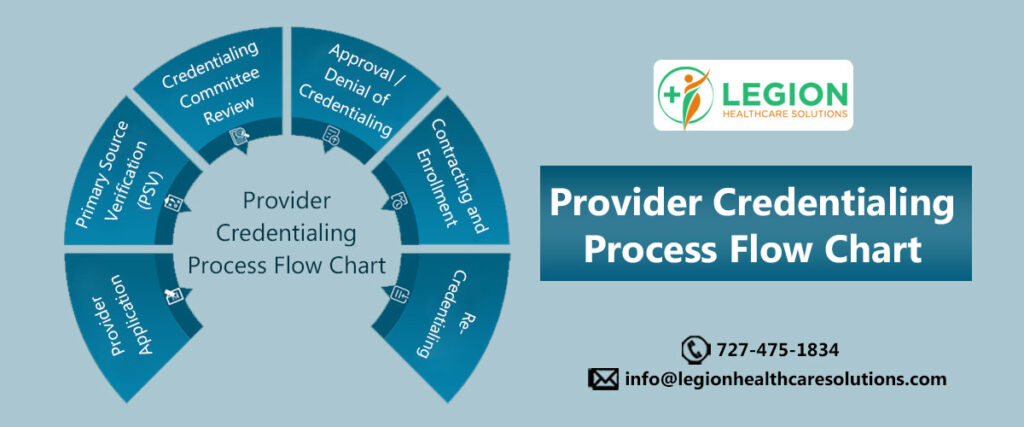
Provider Credentialing Process Flow Chart
Provider credentialing is a critical process in the healthcare industry, which involves the verification of a healthcare provider’s credentials, qualifications, and experience to ensure they meet certain standards set by the insurance companies.
Understanding CPT Code Categories in Pain Management Coding
The use of proper coding categories and codes can help ensure that pain management practices receive appropriate reimbursement for the services they provide.
CareSource Medicaid Prior Authorization – What Providers Need to Know
Prior authorization is a process by which the CareSource Medicaid program reviews and approves certain medical services before they are provided to the patient.
CPT Codes for Active Wound Care Management
Wound care is an essential aspect of healthcare, and the management of wounds requires specialized care to ensure proper healing and prevent infections.
10 Most Common Chiropractic Billing Modifiers
Chiropractic care is a growing industry that is becoming increasingly popular among patients seeking non-invasive treatments for musculoskeletal conditions. However, billing for chiropractic services can be complex and challenging, as it requires a thorough understanding of the codes and modifiers used in medical billing.
Outsourcing Podiatric Medical Billing Services to Legion Healthcare Solutions
As a podiatrist, you know that running a successful practice requires more than just providing excellent patient care. You also need to navigate the complex world of medical billing, from navigating regulations and requirements to submitting accurate claims and appealing denials.
Understanding the Impact of Medicare Carve Out Rule on OB/GYN Providers
The Medicare Carve Out rule can have a significant impact on OB/GYN providers, as many of the services they provide are eligible for carve-out under Medicare regulations.
Demystifying Medicare AWV Coding
Medicare billing can be complex and confusing, especially when it comes to coding for Annual Wellness Visits (AWVs).
Provider Enrollment for Medicaid – Top Trends for 2023
One of the top trends in Medicaid provider enrollment for 2023 is the increased use of technology to streamline the enrollment process. With the rise of digital solutions, providers can now use tools like electronic health records (EHRs) and online portals to automate much of the enrollment process.
Legion – Leading Pain Management Billing Company
Legion Healthcare Solutions specializes in medical billing and revenue cycle management services for pain management practices.
Understanding NCQA Provider Credentialing Standards
The National Committee for Quality Assurance (NCQA) provider credentialing standards are a set of guidelines that insurance companies must follow to ensure […]
Understanding Medicare GY Modifier for Chiropractic Services
The Medicare GY modifier is used to indicate that a service or item is statutorily excluded or does not meet the definition of any Medicare benefit.
Basics of Prior Authorization for Prescription Medications
Prior authorization is a process that healthcare providers must go through before prescribing certain medications or treatments. This process involves obtaining approval from a patient’s insurance company before the medication or treatment can be prescribed.
CMS AWV Guidelines for Primary Care Providers
The Centers for Medicare and Medicaid Services (CMS) publishes guidelines for the AWV on an annual basis, and it’s important for primary care providers to stay up to date on the latest guidelines to ensure that they are properly documenting and billing for the AWV
Understanding UnitedHealthcare Provider Enrollment
UnitedHealthcare is one of the largest health insurance providers in the United States, with millions of members enrolled in their plans. Being a part of their network can help you expand your patient base and increase your revenue.
Legion: Leading Wound Care Billing Company
Wound care providers face unique challenges when it comes to medical billing. Proper coding and documentation are crucial to ensure that claims are processed accurately and efficiently.
Prior Authorization for Prescription: Know the Basics
As a healthcare provider, you know that prior authorization for prescription is a critical step to ensure that patients receive appropriate medications.
Most Common OB GYN CPT Codes
The medical billing and coding process is an essential aspect of healthcare administration that ensures accurate and efficient reimbursement for medical services provided.
Provider Credentialing in Washington State
Provider credentialing is the process of verifying the qualifications, education, and training of healthcare providers, including physicians, nurses, and other allied health professionals, to ensure they meet the standards set forth by insurance companies.
Understanding Provider Enrollment for Aetna
Aetna is one of the largest healthcare insurance providers in the United States. If you are a healthcare provider looking to enroll with Aetna, there are several steps you need to follow.
Procedure Codes for RPM in Pain Management
Remote Patient Monitoring (RPM) has become an increasingly popular way to manage patients with chronic pain. However, there are several insurance reimbursement challenges for RPM in pain management.
Understanding Insurance Prior Authorization Process
The insurance prior authorization process typically begins when a healthcare provider submits a request to the insurance company for a specific medical service or treatment.
Billing for Well Woman Preventive Visit
During a well-woman preventive visit, the healthcare provider typically conducts a comprehensive physical exam and takes a detailed medical history.
Tackling Telehealth Reimbursement Issues
Telehealth reimbursement issues can be complex and vary depending on the specific circumstances and location of the healthcare provider. However, there are some general steps that can be taken to tackle telehealth reimbursement issues.
Reducing AR in Primary Care Practice
While working with various primary care practices, some of the processes contributed more towards reducing accounts receivables. Such processes are discussed in this article.
Legion’s Guide to Provider Credentialing Best Practices
Provider credentialing is the process of verifying and evaluating the qualifications and credentials of healthcare providers, to ensure they meet the necessary standards and regulations for their respective roles.
Avoiding Claim Denials in Wound Care
In wound care, claim denials occur when a healthcare provider’s claim for payment is rejected by the payer, which may be a government program, insurance company, or other third-party payer.
Provider Credentialing Steps in Medi-Cal
Provider credentialing is a process by which a healthcare provider is verified to ensure they meet the necessary requirements to provide healthcare services to patients. Some of the provider credentialing steps in Medi-Cal are discussed in this article.
Improving Pain Management Billing and Coding
Pain management billing and coding requires a high level of expertise and attention to detail to ensure accurate reimbursement and compliance with regulations.
Making Oncology Billing and Coding a Smooth Process
Oncology billing and coding refers to the process of assigning the appropriate medical codes to the procedures and services provided to cancer patients, and submitting claims for reimbursement to insurance companies or government programs such as Medicare and Medicaid.
Challenges of Oncology In-House Billing
Oncology in-house billing refers to the process of billing and collecting payment for oncology services provided by a healthcare facility within the facility itself, rather than outsourcing the billing process to a third-party billing company.
Collecting Deductibles from Patients
In this article, we shared basic tips on collecting deductibles from patients. These tips would be helpful to you immediately as a new year is about to start and deductibles get rest from 1st Jan every year.
Understanding Time Based Evaluation and Management (E/M) Billing Overhaul
In this article, we discussed this time-based evaluation and management (E/M) billing overhaul, focussing on time calculation.
How to Improve Medical Billing Department?
Improving the medical billing department is crucial for the success of any healthcare facility. Efficient medical billing department not only ensures smooth day-to-day operations but also ensures financial sustainability in long term.
Understanding Category G89 Codes for Pain Management
Category G89 includes codes for acute pain, chronic pain, and neoplasm-related pain, as well as codes for two pain syndromes.
Everything You Should Know while Billing for Bariatric Surgery
Bariatric surgery procedures are performed to treat comorbid conditions associated with morbid obesity.
Basics of Preauthorization for DME
Every insurance company has its unique guidelines for preauthorization for DME, still, in this article, we shared the basics of preauthorization for general understanding purposes.
Guidelines for Anesthesia Services Billing
Anesthesia services include, but are not limited to, pre-operative evaluation of the patient, administration of anesthetic, other medications, blood, and fluids, monitoring of physiological parameters, and other supportive services.
Outsourcing can Help Overcoming Revenue Cycle Hurdles
In this article, we will discuss how outsourcing can help overcoming revenue cycle hurdles.
Commonly Used Modifiers for Global Surgeries
Understanding of modifiers for global surgeries, ensures that healthcare organizations are getting paid accurately while billing for all services and without fear of external payer audits.
Billing for Critical Care Visits: Everything You Need to Know
Billing for critical care visits is challenging due to various factors affecting billing scenarios and code selection.
Guidelines for Emergency Department E/M CPT Codes
Any physician seeing a patient registered in the emergency department may use Emergency Department E/M CPT codes i.e., 99281 – 99285.
Understanding Basics of Evaluation and Management Service
Evaluation and management (E/M) procedure (CPT) codes ranges from 99202 to 99499 representing services provided by a physician or other qualified healthcare professional.
Guidelines for Chemotherapy Administration Codes
Chemotherapy administration codes apply to parenteral administration of non-radionuclide anti-neoplastic drugs
Pediatric Audiology Billing Guidelines for 2023
Pediatric audiology billing guidelines can be confusing as it varies from one insurance carrier to another.
Getting Ready for Revenue Cycle Challenges in 2023
In a recent Revenue Cycle Management Virtual Summit, c-suite executives, revenue cycle directors, and other leaders from healthcare organizations discussed the most significant challenges and opportunities in revenue cycle management.
Differentiating Between Medicare Repair and Replacement in DME
DME suppliers often confuse between repair and replacement, making errors while submitting claims to Medicare
4 Key Points in Gastroenterology Billing To Get Reimbursed
Insurance reimbursements are core to any practice’s successful day-to-day operations and Gastroenterology practices are no exception.
Common Hand Surgery Coding Mistakes
Hand surgery coding plays an important role in accurately determining the procedure performed and quantifying the amount of work done by the surgeon.
Watch Out for Claim Denials Pulling Your Practice Down
Claim denials received from government and commercial insurance carriers halt the process of steady insurance collections.
Essentials of Payer Contract Negotiations
Reimbursements are a significant source of revenue for healthcare practices.
Guidelines for Emergency Department Evaluation and Management Codes
The basic requirement for emergency department (ED) is, the facility must be available 24 hours a day.
Understanding Origin and Destination Codes in Ambulance Billing
An important ambulance billing best practice is knowing how to code ambulance transport origins and destinations properly.
Documentation Guidelines for Ultrasound Examination
Accurate and complete documentation and communication by all members of the diagnostic ultrasound health care team are essential for high-quality patient care.
How MPFS is Changing Pain Management Billing for 2023
Let’s understand how MPFS is changing pain management billing for 2023.
Guide to Medicare’s 8-Minute Rule for Physical Therapists
You deserve to be paid for the services you provide in accordance with Medicare’s rules, and we can assist you with that.
Increased Importance of Telehealth Physical Therapy post Pandemic
During a pandemic, telehealth physical therapy has evolved and overcome its limitations.
Timely & Accurate Reimbursements for Wound Care Practice
Major challenge in successfully running a wound care practice is receiving timely and accurate insurance reimbursements.
Common Pitfalls in Cardiology Medical Billing
In this article, we listed common pitfalls in cardiology medical billing, and avoiding them would ensure the financial sustainability of your cardiology practice.
Why Physicians are Outsourcing Medical Billing?
Let’s try to understand why physicians feel outsourcing medical billing services is the right option.
Medicare Coverage Policies for Chronic and Acute Pain
In this article we focussed on Part A and B Medicare coverage policies for chronic and acute pain.
Understanding Basics for Pulmonary Diagnostic Services Coding
Physicians has lot of confusion on how to billing accurately for Pulmonary Diagnostic Services.
Emphasizing Importance of Telehealth for Opioid Use Disorder (Tele-OUD) after COVID-19
Telehealth is a promising approach to increase availability and reach of treatment services, and use and interest has grown for telehealth-delivered treatment of OUD since the COVID-19 pandemic.
Permitted CPT Codes for Physical Therapy
Physical Therapists (PTs) spend countless hours working with clients to rehabilitate and strengthen them after injury.
Everything You Need to Know About E/M Documentation
A significant portion of your practice’s billable services are comprised of evaluation and management (E&M) services.
Understanding Basics of Polysomnography and Sleep Testing Billing
About 40 million people in the United States suffer from sleep problems every year.
Guidelines for Telebehavioral Health Billing Prior Pandemic
In this article, we shared guidelines for telebehavioral health billing which included discussing the place of service (POS) codes, applicable modifiers, and procedure codes.
Unique Challenges of Cardiology Medical Billing
Cardiology medical billing offers unique challenges as various sub-specialties of cardiology are involved.
Perks of Outsourcing Billing for Physical Therapy Services
Physical therapy is becoming more important for practices and healthcare organizations than ever before.
Guidelines for Chemotherapy Administration Codes
Chemotherapy administration codes apply to the parenteral administration of non-radionuclide anti-neoplastic drugs, anti-neoplastic agents, or substances such as monoclonal antibody agents, and other biologic response modifiers.
Understanding Ambulance Transport Coverage Scenarios
Ambulance transportation involves various destination scenarios where beneficiary is transported from beneficiary home, an accident scene, or any other point of origin
Understanding Basics of EDI Enrollment
Electronic Data Interchange (EDI) is an innovative digital communication tool that is used to deliver data from a provider to a payer.
Revised Guidelines for ICD-10 Oncology Coding
Many of the guidelines updated for 2022 focus on the need to code the diagnosis to the highest level of specificity.
Proposed Billing Guidelines for Opioid Treatment Programs
In July 2022, CMS proposed Medicare Physician Fee Schedule Proposed Rule for the year 2023. We discussed the revised billing guidelines for Opioid Treatment Programs proposed in this rule.
Getting Reimbursed for Physical Therapy Services
Getting reimbursed for physical therapy services is challenging but not difficult, focussing on key areas like skilled level of service, medical necessity, and supporting documentation will ensure accurate insurance reimbursements.
Understanding Provider Credentialing Process
For understanding the provider credentialing process in detail and to remove any confusion, experts here at Legion Health Care Solutions shared step by step guide on provider credentialing.
Perks of Outsourcing Medical Billing Services
Next-gen practice owners are outsourcing their complete medical services.
Understanding Key Medical Billing Metrics
In this article, let’s understand the key medical billing metrics and how tracking them could help in increasing your practice collections.
Tips to Improve Your Practice Collections
Medical billing and coding require an in-depth understanding of billing terminologies, state-specific billing and coding guidelines, insurance carrier reimbursement policies, medical specialty-wise insurance coverage, and many others.
Understanding Medicare Part A, B, and D Coverage
In this article, we shared basics of Medicare coverage and services covered under every plan. It will help providers and billers to collect accurate patient responsibility at the time of service only.
Improving Revenue Cycle Management of Healthcare Practice
Efficient revenue cycle management is essential for healthcare practice to operate successfully.
5 Essential Medical Billing Reports for Your Practice
Managing claim denials is the most challenging part of revenue cycle management for any healthcare practice.
Understanding Most Common Denials in Medical Billing
Managing claim denials is the most challenging part of revenue cycle management for any healthcare practice.
Role of Prior Authorization in Medical Billing
Prior authorization (or pre-authorization) is usually required if the patient needs a complex treatment or prescription.
How Does a Radiology Medical Billing Services Provider Help a Radiologist?
Let us understand how a radiology medical billing service provider helps a radiologist do his work in a better fashion.
Why Does a Skilled Nursing Facility Require a Medical Billing Service Expert?
Pediatricians need to have calm and patient composure. The main reason for this is that they deal with children. These children are just born. Similarly, they can be children of very young dispositions.
Why is Pediatric Medical Billing So Important for Pediatrics?
Pediatricians need to have calm and patient composure. The main reason for this is that they deal with children. These children are just born. Similarly, they can be children of very young dispositions.
What Is The Role Of Optometry Medical Billing Services Provider?
Optometry is the branch of science that studies vision, its phenomena, and diseases. Optometrists are also known as ophthalmologists or doctors of optometry.
How Does a Podiatry Medical Billing Service Provider Help a Podiatrist?
A number of insurance companies neglect podiatric services. In fact, insurance companies do not cover many important podiatric services. The main reason for that is that they handle and take care of illnesses that are concerned with the feet and other ailments.
Why Do CPT Codes In Cardiology Medical Billing Require Special Attention?
There are many different medical treatments. However, treatments that are related to cardiology are one of the most expensive. Right from the beginning, these treatments are costly.
Why Are Wound Care Billing Services Important?
People say that time heals all wounds. However, in reality, every wound, be it a small or large one, needs to be treated on time.
How Do OB-GYN Medical Billers And Coders Help Practices?
Childbirth is a miracle for the very reason that the mother puts her own life on the line to bring forth her little one into the world. OB-GYN practitioners make this miracle possible through their flawless services.
What are the Ways Family Practice Billing Services Provider Helps to Increase Medical Practice Revenue?
Family Practitioners are the doctors who treat every member of the family. They treat them irrespective of disease, gender, and age. Family practitioners are also known as family physicians or family doctors.
How can Durable Medical Equipment Billing Companies Relieve Doctors from Medical Equipment Concerns?
Doctors toil to listen to their patient’s concerns and identify the kind of medical issues patients face. And treat them. However, in some cases, doctors are unable to complete treatments because they require medical equipment.
Why Outsourcing Chiropractic Billing Services is a Positive Step for Chiropractors?
Do you have a chiropractic practice? If yes you would understand how difficult it is to take care of your patients. In a similar manner, it is difficult to check the finance and administration issues and run errands for the practice. This article is about how Outsourcing Chiropractic Billing Services can be of some help to the practice?
How Does Dermatology Medical Billing Company Assist A Dermatologist In Better Dermatology Revenue Cycle Management?
Dermatology is the study of treatment and diagnosis of issues related to skin, hair, nail, or mucous membrane. A dermatologist is a doctor who treats the above health issues.
Why Do Cardiology Specialties Require A Cardiology Medical Billing And Coding Service Provider?
A Cardiology expert treats all kinds of diseases that relate to the heart and blood vessels. A cardiologist’s work is complex. In a similar manner, Cardiology Medical Billing is also complicated. This often leads to the denial of claims.
Why Does A Dental Practice Require A Skilled Dental Billing Service Provider?
In the United States, a majority of people have insurance cover for dental treatments. Dental Medical Billing and Coding are related to dental care. In this article, we will understand why a dental practice should take the help of a skilled Dental Billing Services provider.
What Are The Advantages Of Outsourcing Oncology Medical Billing?
Cancer has become one of the fastest-spreading diseases nowadays. It is even termed one of the deadly diseases. The study of cancer is called Oncology Medicine. On the other hand, Medical Oncology Billing is the process to convert these services into codes that an insurance company understands.
How Will State Budget Cuts On Mental Health Affect Mental Health Medication Management?
What will happen if you give a group of people all the work? The result is that their focus would divert, right? Correspondingly, won’t this will lead to a lack of expertise in work? Moreover, it will even cause delays in the end result.
How Does Medical Billing And Coding In Florida Help A Medical Or Dental Practice In That State?
Florida has one of the highest-ranked hospitals, medical practices, and dental clinics in the United States. They are one of the most sought-after ones because of the service they offer their patients. The sad part is that even though the state has one of the highest-ranked hospitals and medical practices, the condition of the payment is on a decline. This article sheds light on how Medical Billing and Coding in Florida can usher the way for a better income for the services.
Why Is The Credentialing Process Crucial For The Healthcare Industry?
Credentialing is the process to understand the capabilities of licensed clinical experts. Similarly, it also evaluates their experience and capabilities. This article points out the reason why credentialing is important. It also points out how a Credentialing Process Provider can assist a medical practice or hospital.
How can An Improved Orthopedic Collection Process Be Helpful for a System?
Orthopedic Medical Billing systems are essential for regular movement in everyday life. The orthopedic billing substantially depends on proper attestation before, during, and after the case’s visit.
Why Choose to Outsource Medical Billing Services
What will happen if you give a group of people all the work? The result is that their focus would divert, right? Correspondingly, won’t this will lead to a lack of expertise in work? Moreover, it will even cause delays in the end result.
How to Execute a Robust Pain Management Collection System
Pain management collection is a very dynamic field. The reason is that the ICD codes are complex. Moreover, the payer’s demands also change from time to time. Due to these reasons, it becomes inevitable that we have an effective Pain management collection system.
What is the Difference Between Medical Billing and RCM?
At their core, Medical Billing Services and revenue cycle management solutions aim to facilitate the collection of financial data from healthcare providers. […]
Things You Will Learn About Ambulance Billing Service And Its Functionality.
Emergency Billing Service helps ambulance companies maximize earnings with a minimum time-out. They specialize in preparing documentation to get checks paid, make […]
Telemedicine Billing: What every Physician should know?
Physicians decreasing revenue and patient volume is negatively impacting most practices in the country. Physicians need innovation in practice to fulfill their […]
Outsourcing your Medical Billing: What questions should ask before selecting a Medical Billing Company?
Medical practitioners in the country see a steady drop in revenue; with a pandemic, the situation became grave with reduced volume. According […]
Physician Credentialing: What every Physician should know about?
Physician Credentialing or Doctor Credentialing or Medical Credentialing or Provider Credentialing names can be different but with same process. Every healthcare professional […]